Diabetes and Metabolic Imbalances
Between 1980 and 2009, the number of diagnosed diabetes cases in the U.S. tripled. Today, the CDC estimates that over 25 million people—approximately 1 in every 12 Americans—have diabetes. Additionally, 1 in 3 adults over the age of 20 shows symptoms of prediabetes. Despite public health efforts, dietary recommendations such as the USDA’s former Food Pyramid and current Food Plate are based on outdated science and a poor understanding of nutrition. As a result, these guidelines have inadvertently contributed to the rise of obesity and chronic disease, with diabetes leading the charge.
Understanding Diabetes
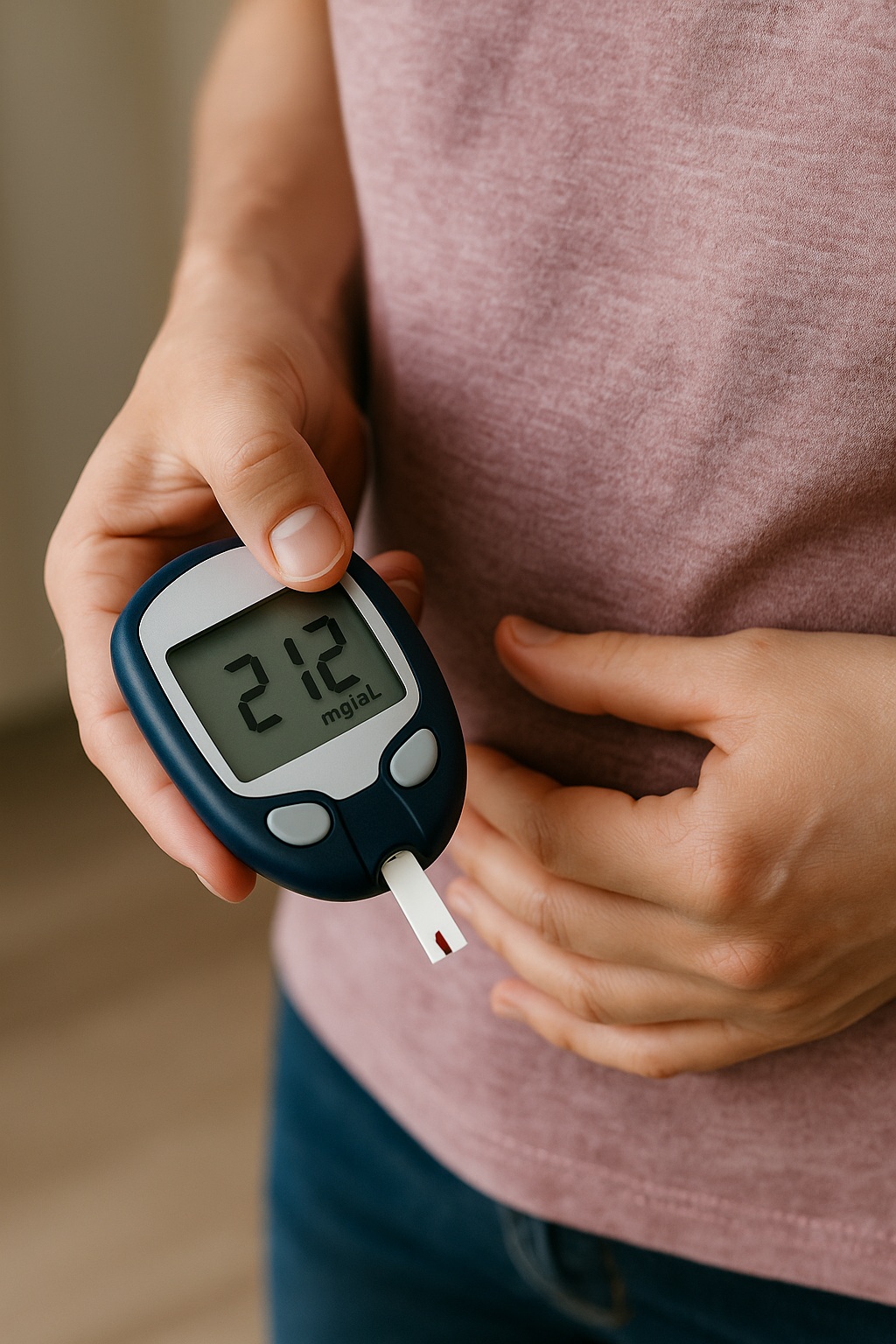
Diabetes is a condition characterized by elevated levels of glucose in the blood. Glucose, the body’s primary energy source, is transported into cells by insulin, a hormone produced by the pancreas. In Type I diabetes, an autoimmune process destroys the body’s insulin-producing cells. In contrast, Type II diabetes, which accounts for 95% of all cases, develops when the body becomes resistant to insulin. Over time, the pancreas may also fail to produce enough insulin, leading to chronically high blood glucose levels.
Consequently, in both Type I and Type II diabetes, glucose cannot effectively enter cells. The body behaves as if it were starving, resulting in symptoms such as extreme thirst and hunger (especially for sweets), fatigue, and frequent infections. If left unmanaged, advanced diabetes can cause severe complications, including kidney failure, amputations due to tissue necrosis, and even blindness. While Type I diabetes tends to appear suddenly, Type II usually develops gradually over several years.
Reactive Hypoglycemia
Reactive hypoglycemia refers to abnormally low blood glucose levels. Symptoms often include dizziness, shakiness, confusion, and in severe cases, seizures or coma. Milder symptoms are common and may occur when meals are skipped or lack adequate protein and fat. Notably, hypoglycemia triggers the adrenal glands to release cortisol, activating the body’s stress response.
Insulin Resistance
Insulin resistance describes a state in which cells become less responsive to insulin, thereby impairing the body’s ability to lower blood glucose effectively. This condition often precedes the development of Type II diabetes.
Clinical Progression and Management
From a clinical standpoint, metabolic disorders typically follow a progression—from reactive hypoglycemia, to insulin resistance, and finally to full-blown diabetes. Each stage has distinct symptoms and identifiable blood markers. Early recognition and proper nutritional management are therefore crucial to prevent disease advancement.
If diabetes is already diagnosed, management should focus not only on blood sugar control but also on addressing secondary complications. The following integrative therapies have shown potential:
- Acupuncture: Supports immune function, promotes circulation, reduces stress responses, alleviates pain, and helps regulate blood sugar.
- Dietary Counseling: Focuses on nutrient-dense, individualized diets based on scientific evidence, to reverse metabolic dysfunction.
- Herbal and Nutritional Supplementation: Aims to improve glucose regulation, hormone balance, immune strength, and organ system resilience.
Supporting Evidence
Multiple peer-reviewed studies have explored these approaches:
- Robeva R, et al. J Pineal Res. 2008;44(1):52–6.
- Davis SN, et al. J Clin Endocrinol Metab. 2011;86(5):2043–50.
- Davis SN, et al. Diabetes. 1997;46(8):1328–35.
- Burge et al. J Clin Endocrinol Metab. 2001;86(11):5471–8.
- Scott & Scandart. Diabetes Care. 1981;4(5):514–8.
- McGregor et al. Am J Physiol Endocrinol Metab. 2022;282(4):E770–7.
- Davis et al. J Clin Invest. 1997;100(2):429–38.
- Widdowson PS, et al. Diabetes. 1997;46:1782–85.
- Bosi E, et al. Diabetologia. 2006;49(12):2824–7.